ترجمه فارسی عنوان مقاله
تحویل اصلی بزرگسالان درمورد ناهنجاری های آئورت بطنی نزولی
عنوان انگلیسی
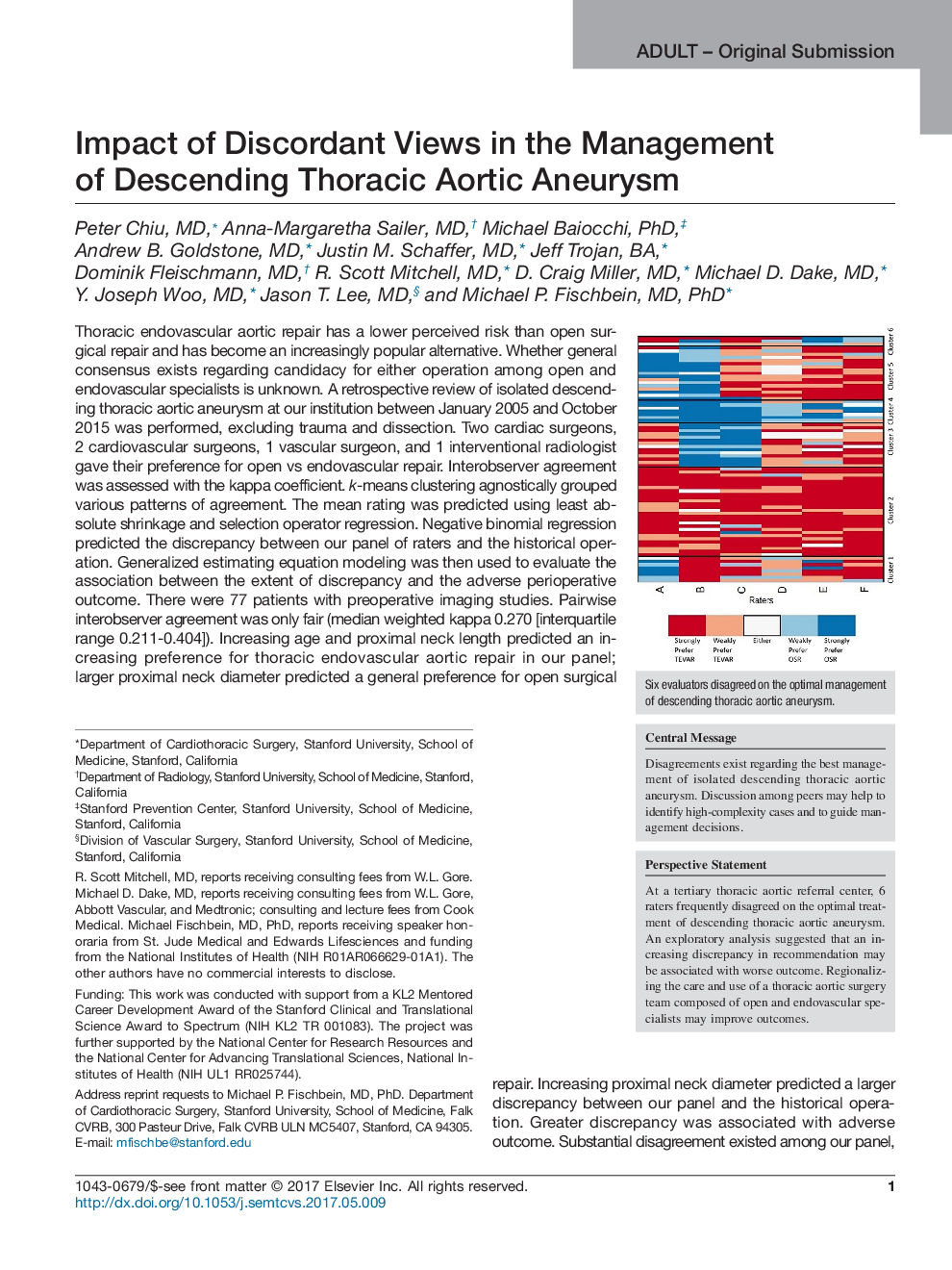
Adult Original SubmissionImpact of Discordant Views in the Management of Descending Thoracic Aortic Aneurysm
| کد مقاله | سال انتشار | تعداد صفحات مقاله انگلیسی |
|---|---|---|
| 161921 | 2017 | 9 صفحه PDF |
منبع

Publisher : Elsevier - Science Direct (الزویر - ساینس دایرکت)
Journal : Seminars in Thoracic and Cardiovascular Surgery, Volume 29, Issue 3, Autumn 2017, Pages 283-291